Disposition Appendix: Synopsis from Science & Benchmarking Supporting REGDOC-2.2.4, Fitness for Duty, Volume I: Managing Worker Fatigue
Contents
1.0 Background
Human performance is a key contributor to the safety and security of nuclear facilities, so the CNSC requires licensees to implement and maintain human performance programs. These programs address a broad range of factors that affect human performance, with the aim of minimizing the potential for errors that could affect nuclear safety and security. One of these factors is a worker’s fitness for duty.
Fatigue is widely recognized to affect fitness for duty because of its potential to degrade several aspects of human performance. Therefore, licensees must address fatigue as part of their approach to ensure that workers are fit for duty.
REGDOC-2.2.4, Fitness for Duty, Volume I: Managing Worker Fatigue, specifies requirements and gives guidance for managing worker fatigue with the aim of minimizing the potential for errors that could affect nuclear safety and security. Managing worker fatigue encompasses measures to manage risks associated with fatigue, including measures to manage the level of fatigue that workers experience at work and to reduce the likelihood and consequences of fatigue-related errors (1). For the purpose of the regulatory document (REGDOC), fatigue is defined as a state of reduced mental or physical performance capability resulting from sleep loss, extended wakefulness, phase of the circadian rhythm, or workload.
The purpose of this synopsis of science and benchmarking is to inform the Commission and to address a range of comments received during public consultation. The REGDOC has been modified to address many concerns raised by stakeholders during public consultation about operational needs and administrative burden while maintaining a basis that is defensible based on benchmarking and on scientific research about the effects of fatigue on human performance. The limits on hours of work and recovery periods in Section 4 of the REGDOC have been reviewed against scientific research, compared to requirements of other regulatory bodies, and tested using a bio-mathematical fatigue model. Independent research reports commissioned by the CNSC over several years have been considered in the development of this REGDOC (2; 3; 4).
The following findings regarding the effects of fatigue on human performance form the basis for the provisions in the REGDOC.
1.1 Fatigue Affects Human Performance
- Declines in human performance occur whether fatigue is related to acute sleep deprivation, cumulative sleep deprivation, or the circadian rhythm.
- Acute fatigue is caused by extended hours awake, with fatigue levels increasing with the time since the last sleep episode (5).
- Cumulative fatigue is caused by mild sleep restriction over a series of days that results in insufficient recovery from acute fatigue (6; 7; 8).
- The circadian rhythm of the sleep/wake cycle causes fatigue levels to vary throughout the day with the greatest levels of fatigue in the early hours of the morning (5).
- Negative effects on human performance increase further when multiple factors that contribute to fatigue are present, such as working at 4 a.m. after a period of extended wakefulness and/or consecutive days of sleep restriction (9; 10).
- As fatigue increases, degradation occurs in many aspects of human performance (11; 12; 13; 14; 15; 16; 17; 18). Examples of abilities affected include the following: vigilance (19; 6; 20; 21; 22; 7; 23; 13); memory (21; 24; 25; 13; 26); decision making (27; 28); communication (27); anxiety (29; 23); mood (21; 16; 23).
- A review of the effect of sleep deprivation on decision-making highlights the following areas of concern: lack of innovation, inflexibility of thought processes, inappropriate attention to peripheral concerns or distraction, over-reliance on previous strategies, unwillingness to try out novel strategies, unreliable memory for when events occurred, change in mood including loss of empathy with colleagues, and inability to deal with surprise and the unexpected (27 p. 246).
- The range of cognitive abilities affected implies that fatigue "impairs some essential capacity that is basic to cognitive performance in general" (30 p. 654). The fatigue-related change in cognitive function has been described as "cognitive slowing" (20).
- Fatigue "...is not a binary condition in which one is either rested with no negative effects on performance or fatigued with severe negative effects on performance. There are degrees of fatigue and degrees of the negative effects of fatigue on performance" (31 p. 12). The "more sleep is disturbed or reduced, for whatever reason, the more likely an individual will inadvertently slip into sleep" (32 p. 102).
- A review of aviation maintenance events found that the frequency of skill-based errors follow the circadian rhythm with a peak between 02:30 and 03:00. The authors caution that "maintenance technicians are at heightened risk of 'absent minded' errors involving failures to execute action plans as intended" in the early hours of the morning (33 p. 1304).
- Nuclear workers in Canada experience sleep loss, fatigue and fatigue-related symptoms that are similar to those discussed in scientific literature (2; 34).
2.0 Rationale for Requirements and Guidance in REGDOC 2.2.4
The requirements and guidance in the REGDOC are presented in two sections. Programmatic elements are in Section 3 and prescriptive limits on hours of work and recovery periods are in Section 4 of the REGDOC.
Programmatic elements in Section 3 are applicable to the broad population. The broad population includes workers who have the potential through their work activities to pose a risk to nuclear safety or security.
Limits on hours of work and recovery periods in Section 4 are applicable to a smaller subset of workers who fill safety-sensitive positions (SSPs). A SSP is defined as a "position which has a role in the operation, where impaired performance could result in a significant incident affecting the environment, the public, the health and safety of workers and others at site, or the safety and security of the facility". Most of the limits on hours of work and recovery periods in Section 4 focus on night work and extended shifts longer than 10 hours, which are features of the work schedule widely recognized to contribute to fatigue.
The rationale for requirements and guidance in the REGDOC is outlined in the following sections.
2.1 Programmatic Elements
Workplace fatigue is a potential risk that needs to be managed, especially in 24/7 operations that require work schedules that interfere with sleep (e.g., extended shifts, rotating shifts, night shifts) (30; 4; 35). In addition to measures that reduce the occurrence of fatigue, additional fatigue mitigation strategies are needed to reduce the likelihood and consequences of fatigue-related errors (35; 8; 36; 37). A third-party review conducted for the CNSC recommended that the effectiveness of hours of work and recovery requirements could be augmented through implementation of fatigue risk management systems (4).
Even when complying with limits on hours of work, a worker may be fatigued. Since factors at work and outside of work affect fatigue, workers share responsibility with the employer for managing fatigue.
Programmatic requirements and guidance in the REGDOC address a broad range of elements necessary for managing fatigue-related risks (8; 36; 38; 39; 40). The conceptual framework in Figure 1 provides an overview of multiple barriers against fatigue-related errors that are captured in the REGDOC (36). For the purpose of the REGDOC, managing worker fatigue encompasses measures to manage the level of fatigue that workers experience at work and to reduce the likelihood and consequences of fatigue-related errors.
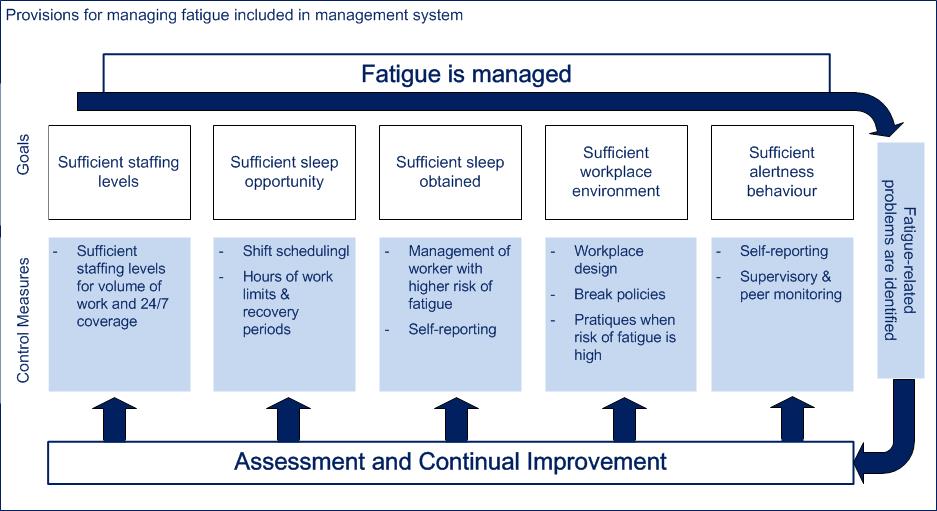
Figure 1: Conceptual framework supporting provisions for managing worker fatigue [based on Reference 36]
Staffing levels, which affect overtime levels, are an important contributor to fatigue (36; 3). A research report conducted for the AECB cautions that understaffing "is likely the largest contributor to fatigue levels in continuous operations. An understaffed operation typically results in high levels of employee overtime, thus reducing the amount of rest days and contributing to fatigue" (3 p. 14). As part of the programmatic elements, the REGDOC requires licensees to conduct periodic assessments to verify that staffing levels are sufficient for enabling adherence to limits on hours of work and recovery periods.
Work schedules established by the organization affect the sufficiency of sleep opportunities because they define the boundaries for the timing and duration of sleep (41). Key aspects of a work schedule that affect sleep opportunities are night work and the duration, frequency, and sequencing of successive shifts. Section 2.2 provides more information about the rationale for the REGDOC’s requirements applicable to hours of work and recovery periods.
The sufficiency of sleep obtained is also affected by factors outside of work. For example, certain circumstances or conditions, such as sleep disorders or medical conditions, affect the quality and quantity of sleep a person obtains, and thus, increase the likelihood of people experiencing high levels of fatigue (14; 42; 43; 44; 45). The REGDOC addresses the sufficiency of sleep obtained through processes for identifying and managing fatigue and through expectations for initial and ongoing training and education.
The workplace environment can be designed to promote alertness and to manage risks associated with fatigue. For example, in the middle of the night when high levels of fatigue are expected, additional administrative measures could be implemented, such as increased supervisory oversight and independent verification. Rest periods that include an opportunity for sleep are an evidence-based strategy to reduce fatigue levels and improve human performance (46; 47; 48; 36). The REGDOC clarifies that there are no regulatory impediments to licensees permitting sleep at work as a fatigue countermeasure, as long as appropriate conditions are defined. Section 3.2 of the REGDOC includes guidance related to the workplace environment.
The final barrier in Figure 1 of sufficient alertness behaviour requires supervisors and workers to be aware of signs of high levels of fatigue in themselves and in peers, so appropriate actions can be taken. However, self-identifying high levels of fatigue may be challenging because people may not perceive their performance to be affected by fatigue (7). The REGDOC includes requirements for training and education and for the process to follow if a worker may be unable to competently and safely perform his/her assigned duties because of fatigue.
The REGDOC also includes mechanisms for identifying and resolving problems related to worker fatigue, for determining the effectiveness of the management system in managing the risks associated with worker fatigue, and for identifying opportunities for continual improvement.
2.2 Limits on Hours of Work and Recovery Periods
Work schedules are an important factor when managing fatigue since they define the boundaries for the timing and duration of sleep. For that reason, the REGDOC includes performance-based requirements related to the work schedule applicable to the broad population, which are shown in Figure 2. The time of day when work and sleep occur is an underlying factor that affects all of the performance-based objectives. The intent of the performance-based requirements is to ensure that work schedules provide sufficient sleep opportunities.
The prescriptive hours of work limits and recovery periods in Section 4.2 and 4.3 of the REGDOC specify outer limits applicable to the subset of workers who fill SSPs. The REGDOC also includes guidance stating that licensees should establish administrative limits that prevent workers from consistently working the maximum allowable hours of work.
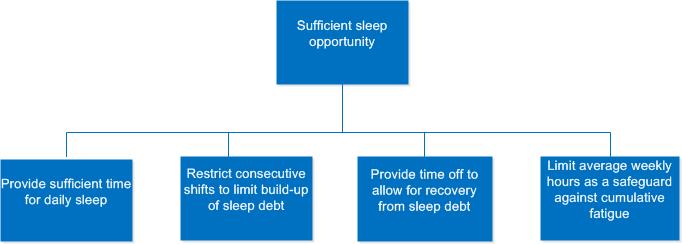
Figure 2: Performance-based objectives supporting provision of sufficient sleep opportunity
The following sections present data supporting each performance-based objective. The performance-based objectives are based on the following scientific findings:
- Cognitive performance varies with the time of day and is lowest at night;
- Extended wakefulness affects cognitive performance;
- Sleep loss across successive days affects cognitive performance;
- Sleep allows the body to recover from fatigue.
2.2.1 Effect of Time of Day on Cognitive Performance
- Circadian rhythms are cyclical changes observed in humans daily across multiple variables, such as temperature, hormones, sleep patterns, and fatigue (15). The circadian system includes an internal circadian pacemaker that is synchronized to the 24-hour day by time cues. A key time cue is light (15).
- Time of day has a powerful effect on human performance, alertness, and sleep propensity.
- The "probability of being asleep is highest during the night-time and lowest during the daytime" (50 p. 654).
- The greatest levels of fatigue occur in the early hours of the morning (5; 21).
- "...the night shift produces the greatest degree of sleepiness relative to daytime work, evening shifts, and even rotating shifts" (21 p. 785).
- The body’s "circadian system strives to keep us asleep at night and awake during the day" (49 p. 553). As a result, fatigue during night shifts is caused by a combination of the circadian low point and obtaining shorter, lower quality daytime sleep than night-time sleep (30).
- The time period from 02:00 to 06:00 is "identified as a time when the body is programmed to sleep and during which performance is degraded" (51 p. 3). In aviation, this time period is commonly known as the “window of circadian low” and additional restrictions apply when work occurs during this time period (51; 52).
- Performance is lower at the end of a 12-hour night shift than at the start of a night shift or at the start or end of a 12-hour day shift (53).
- People can experience drowsiness at any time of the day; however, a study of critical care nurses showed drowsiness and sleep episodes are most likely to occur between midnight and 6 a.m. (54).
- There are cumulative effects when the circadian low coincides with a sleep debt and/or an extended period awake (9).
- A committee reviewing catastrophic events concluded that "inadequate sleep, even as little as 1 or 2 h less than usual sleep, can greatly exaggerate the tendency for error during the time zones of vulnerability" (1 to ∼ 8 a.m.) (32 p. 107).
- The most restrictive requirements in the REGDOC apply to night work due to the increased risk of fatigue.
2.2.2 Sufficient Time for Sleep Daily
The REGDOC includes limits on hours of work for a 24-hour and 48-hour period and a recovery period between shifts. These restrictions are intended to limit extended wakefulness by providing workers with time for sleep daily.
Daily Need for Sleep
- Sleeping less than 7 hours per night is associated with "impaired performance, increased errors, and greater risk of accidents" (55).
- Only a proportion of time free from work is available for sleep. In addition to sleep, workers use time free from work to commute, fulfil family and social obligations, deal with personal needs (e.g., meal preparation, eating, hygiene), and unwind before sleep (56; 57).
- Based on a review of published epidemiologic data on sleep, performance, and motor vehicle accidents, an expert panel established by the National Sleep Foundation Drowsy Driving Consensus Working Group concluded that "[d]rivers who have slept for two hours or less in the preceeding 24 hours are not fit to operate a motor vehicle" (58 p. 96). The panelists also agreed that "most healthy drivers would likely be impaired with only 3 to 5 hours of sleep during the past 24 hours" (58 p. 96).
- The amount of sleep a person obtains is related to the time off between shifts and the time when the recovery period occurs (59).
- People obtain more sleep as the time off increases. For example, as time in bed increases from 4 to 8 hours, so does time asleep (60).
- The duration of sleep is related to the time of day when sleep occurs. Sleep that commences during the day is shorter than sleep that commences at night (61; 59).
- Quick returns, which are defined as less than eleven hours free from work between shifts, are associated with insomnia, reduced sleep quality and duration, and increased fatigue (62; 63; 57).
Effect of Extended Wakefulness on Cognitive Performance
- Short-term total sleep deprivation results in "a significant deleterioius effect across most cognitive domains" (22 p. 384).
- The effect of extended wakefulness can be conceptualized as a build-up of pressure to sleep that is dissipated during periods of sleep (64).
- The longer one has been awake, the greater the likelihood of experiencing fatigue (5).
- Some studies show that shifts that extend beyond 8 hours are associated with a higher level of fatigue and a lower level of performance than 8-hour shifts (65; 66). A review of 105 studies focused on the effects of 8 versus 12-hour shifts concluded that only "with appropriate planning, structuring and proper allowance for rest…may extended work shifts be considered acceptable" (67 p. 132).
- Studies consistently show marked declines in human performance after approximately 17 to 18 hours awake (68; 69; 70).
- Vigilance tests show increases in performance variability after 18 hours awake with "normal short reaction times intermixed with both long-duration lapses (i.e., errors of omission) and responses when no stimulus was present (i.e., errors of commission)" (69 p. 263).
- Failures to respond to stimuli for 30 seconds, which are known as micro-sleeps, begin to occur after 18 hours awake (70).
- A research report prepared for the AECB states that "there is clear evidence in the literature on hours of work that obvious deterioration starts to set in after 14 – 16 hours work. An overtime policy that allowed work to exceed 16 continuous hours would not be a safe one" (2).
- The effect of sleep deprivation is magnified when time awake coincides with the circadian low point during night shifts (10).
2.2.3 Limit the Build-up of Sleep Debt
When people get less sleep than they require over consecutive days, a sleep debt accumulates. People tend to sleep less when working night shifts than day shifts, so the sleep debt accumulates faster when night shifts are worked. Performance declines are proportional to the accumulated sleep debt.
Effect of Sleep Loss Across Successive Days on Cognitive Performance
- A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society states that sleeping less than 7 hours per night is associated with "impaired performance, increased errors, and greater risk of accidents" (55).
- People sleep less on work days than on days free from work (71; 56; 72; 73).
- Several studies show many shift workers sleep less than 6 hours per 24-hour period on work days, especially those working nights and/or extended shifts (74; 75; 76; 77; 78).
- When people get less sleep than they require over consecutive days, a sleep debt accumulates.
- Performance declines accumulate across consecutive days when time in bed is restricted to 7 hours or less (7; 6). The declines in human performance are proportional to the accumulated sleep debt (79; 7; 6; 80).
- A study in which sleep periods were limited to 4 or 6 hours per night for 14 nights found progressively eroded "effectiveness of psychomotor vigilance performance, working memory performance and cognitive throughput performance, providing convergent evidence for the adverse effects of chronic sleep restriction on cognitive functions" (7 p. 124).
- Even though performance declines across consecutive days of sleep restriction, subjective ratings of sleepiness do not increase across consecutive days (7). As a result, people may feel they have adapted to chronic sleep restriction even as their performance declines.
- Data shows that injury and accident risk increase with successive shifts for both day and night shifts (66).
- Longer sequences of consecutive shifts lead to more fatigue (81). The increase in risk is greater across successive night shifts than day shifts (82).
Effect of Sleep Loss Across Consecutive Night Shifts on Cognitive Performance
- Fewer consecutive nights shifts are permitted due to the increased fatigue that is known to accumulate when working at night.
- "Sleep loss accumulates and its impact grows over successive night shifts. The result is a buildup of homeostatic sleep debt combined with the effects of circadian misalignment, with both having serious implications for productivity and safety in shift workers" (83 p. 785).
- "...chronic sleep loss increased the rate of deterioration in performance across wakefulness, particularly during the circadian 'night'" (9).
- "...sleep debt that builds up after a sequence of night shifts supports limiting the number of consecutive night shifts to allow time for recovery" (4 p. 22).
2.2.4 Recovery from Sleep Debt
Recovery periods enable people to recover from the sleep debt that has accumulated over successive shifts. The recovery period following night shifts also accounts for the circadian re-adjustment required to return to a day schedule.
Recovery from sleep debt
- Minimum recovery periods are intended to provide workers with time to recover from the sleep debt that has accumulated over successive shifts.
- Recovery from fatigue, particularly recovery of cognitive function, requires sufficient, good quality sleep (8; 19).
- The amount of sleep a person obtains is related to the free time available for sleep and the time of day when sleep commences (84; 73).
- If recovery periods are insufficient following nights of sleep loss, fatigue and fatigue-related performance decrements can remain at the start of a new shift sequence (85; 19).
- Both day workers and shift workers sleep more on non-work days than on work days on average (71; 56).
- Shift workers are more likely than non-shift workers to sleep less than 6 hours on work days (56).
- A third-party report prepared for the AECB states that as "employees work overtime as an alternative to receiving planned rest days, less opportunity occurs to restore ongoing sleep debts" (3 p. 15). This report also recommended that "a shiftworker should be scheduled to work no more than seven 8-hour shifts before receiving a day of rest" (3 p. 13).
Recovery from sleep debt following night shifts
- The recovery period following a sequence of night shifts needs to account for the sleep debt that has accumulated and the circadian readjustment that is required when switching between night and day shifts (2; 86; 87).
- When Ontario Hydro transitioned to 12-hour shifts, they conducted a study focused on the effects of a 72-hour recovery period following 3 or more night shifts versus a 48-hour recovery period (88). The study concluded that "alertness levels after 48 hours off work are significantly lower than those found after 72 hours off work". In addition, sleep "records suggest a sleep deficit remaining after 48 hours off work". Following this study, Ontario Hydro adjusted station schedules to include a “72-hour break from work after three or more consecutive night shifts” (88).
- Permanent night-shift systems do not lead to sufficient circadian adjustments for most individuals to benefit with respect to health and safety (89).
- "...workers are unlikely to maintain a daytime sleep schedule on their days off" (4 p. 30), which limits their ability to adjust to permanent night shifts.
2.2.5 Limit Average Weekly Hours
As the hours worked in a week increase, opportunities for recovery decline. Weekly limits, as well as longer term limits, provide a safeguard against cumulative fatigue.
Limit weekly hours as a safeguards against cumulative fatigue
- People who work longer hours per week are more likely to sleep fewer hours per day (71; 90; 56). For example, Hale found that those who work more than 50 hours per week have an increased risk of sleeping less than 6.5 hours per day compared to people who work less than 35 hours per week (2005).
- Longer work weeks are associated with an increased risk of
- occupational injuries (91; 92; 93; 94);
- accidents (95; 66); and
- errors (96; 97; 98).
- A study found that those involved in sleep-related vehicle crashes were more likely to work 60-hours per week and/or night work or other schedules (e.g., rotating shifts; long hours for an extended period of time) than controls who had not been in a vehicle crash (95).
- A research report for the CNSC recommended a rolling limit of 60 hours in a 7-day period (4).
Longer term limits to weekly hours
- Longer term limits provide a safeguard against cumulative fatigue while allowing some short-term scheduling flexibility (99).
- A review of hours of work limits for the European Commission recommends "short reference periods for calculating averages of the exposure to work, in order to avoid any undue accumulation of impairing effects during times with high workload or extended hours within the reference period" (100 p. 34).
- The United States (US) Nuclear Regulatory Commission (NRC) noted that security personnel "questioned their readiness and ability to perform their required job duties because of the adverse effects of cumulative fatigue" following the attacks of September 11, 2001. A review by the NRC "confirmed that the individuals had been working up to 60 hours per week for extended periods" (101 p. 17135).
2.2.6 Benchmarking Data
CNSC staff reviewed regulatory requirements from nuclear regulators internationally and from a range of other industries, including aviation, road transport, petrochemical, and pipelines. Direct contact was made with nuclear regulators from several countries (e.g., US, United Kingdom (UK), Romania, China, Korea, Switzerland, France, Sweden, Finland) as well as with Transport Canada and NAV Canada.
Tables 1 to 3 include some of the benchmarking data considered.
Some trends observed in the benchmarking data are as follows.
- The European Union’s (EU) Working Time Directive includes comprehensive limits on hours of work and recovery periods that are applicable in all EU countries. Rather than the nuclear regulators in Europe developing their own requirements related to fatigue management, they tend to rely on national requirements applicable to all workers. In contrast in Canada, there is no national baseline standard applicable to all licensees regulated by the CNSC.
- Most jurisdictions require workers to have 8 to 11 hours free from work within a 24-hour period or between shifts (see Table 1).
- Very few jurisdictions have a limit on hours worked in a 48-hour period. The rationale for this limit in the REGDOC is preventing two consecutive 16-hour shifts. The US NRC, which also requires a minimum recovery period of 8 hours between shifts, also has a limit applicable to a 48-hour period.
- Many jurisdictions have a limit on average weekly hours calculated over a specified period of time.
- The EU Working Time Directive requires member countries to ensure that "the average working time for each seven-day period, including overtime, does not exceed 48 hours" with a reference period for averaging that cannot exceed 4 months. Therefore, workers in European nuclear facilities have this limit in place or one that is more restrictive (e.g., UK Working Time Regulations – 48 hours per week averaged over 17 weeks; Romanian Labour Code – 48 hours per week averaged over 3 months; France Code du travail – 46 hours per week averaged over 12 weeks).
- A requirement for one day off per 7-day period is common internationally (102).
- Several jurisdictions apply additional restrictions to night work. For example, the EU Working Time Directive requires that "normal hours of work for night workers do not exceed an average of eight hours in any 24-hour period" (103).
- The International Labour Organization (ILO) recommends that when shift work involves night work, "a rest period of at least 11 hours between shifts should be guaranteed as far as possible" (104).
- The limits on hours of work applicable to pilots in the Canadian Aviation Regulations, which were published in 1996, are currently undergoing review and update (105). This update will address the International Civil Aviation Organization’s fatigue management standards and recommended practices, which were published by in 2011 (38).
Hours of Work Limits Applicable to High-Security Sites from Other Jurisdictions
- Legislation in Ontario, New Brunswick, and Canada require a weekly rest period of at least 24 consecutive hours. However, employment standards legislation does not differentiate between working days or nights or working standard 8-hour shifts or extended 12-hour shifts.
- While the Ontario Employment Standards Act and Canada Labour Code include limits on daily and weekly hours of work, the New Brunswick Employment Standards Act states that "there is no limit on the number of hours an employee may work during any daily, weekly or monthly period" (section 14).
Table 1: Benchmarking of daily limits and recovery periods in other jurisdictions
| Legislation | Types of Workers | 24-hour limit | 48-hour limit | Recovery Periods | |
|---|---|---|---|---|---|
| (hours af work) | Time off/24 hours | Time off between shifts | |||
| EU Working Time Directive | All workers in Europe, including nuclear | N/A1 | N/A | 11 | N/A |
| Code du travail | All workers in France, including nuclear | 12 | N/A | 11 | N/A |
| Ontario Employment Standards Act | All workers in Ontario (except those exempted) | N/A | N/A | 11 | N/A |
| Canadian Aviation Regulations (CARS) | Canadian pilots – large carriers | 14 | N/A | N/A | 82 |
| Commercial Vehicle Drivers Hours of Service Regulations | Motor carrier drivers (Canada, south of 60o) | 14 | 26 | 10 (8 must be consecutive) | N/A |
| US NRC – 10 CFR Part 26 | US nuclear workers | 16 | 26 | N/A | 8 |
| In REGDOC-2.2.4, Volume I | SSPs, high-security sites | 16 | 28 | N/A | 83 |
| US Federal Aviation Administration (FAA) – 14 CFR Part 117 | US pilots | 9–144 (19) | N/A | N/A | 10 |
1N/A indicates that the legislation does not include this requirement
2Canadian pilots shall be "provided with an opportunity to obtain not less than eight consecutive hours of sleep in suitable accommodation, time to travel to and from that accommodation and time for personal hygiene and meals"
3Guidance in draft REGDOC: A worker should normally be given 11 consecutive hours free from work between shifts. A recovery period of 8 hours should be rarely used (for example, if necessary to fill a minimum staff complement position; when the recovery period occurs at night when the body’s circadian rhythm promotes sleep).
4Permissible flight duty period for US pilots is dependent upon start time and number of flight segments; if certain conditions are met (e.g., augmented crews, bunks, in-flight sleep opportunities), permissible flight duty periods may increase up to 19 hours.
Table 2: Benchmarking of longer-term limits
| Legislation | Types of Workers | Hours/Week | Short-term | Year |
|---|---|---|---|---|
| Loi fédérale sur le travail dans l’industrie, l’artisanat et le commerce | All workers in Switzerland, including nuclear | 49 (temporarily, otherwise 45) | N/A5 | 140 hrs. overtime |
| Code du travail | All workers in France, including nuclear | 60 (with authorization) | 46 hours/week (with authorization) averaged over 12 weeks (44 for nights) | 1607 hrs. |
| Romanian Labour Code | All workers in Romania, including nuclear | 48 (may be averaged over 3 months) | 48 hours/week averaged over 3 months | N/A |
| US – 14 CFR Part 117; EU Commission Regulation 859/2008 (EU OPS) Subpart Q6 | US & EU Pilots | 60 hours7 | 47.5 hours/week averaged over 4 weeks (190 hrs flight duty time in 28 days) | N/A |
| CNSC – in REGDOC-2.2.4, Volume I | SSPs, high-security sites | 60 hours in a fixed 7-day period or 120 hours in a rolling 14-day period | 54 hours on average over a fixed 13-week period or 18-week rolling period | N/A |
| US NRC – 10 CFR Part 26 | US nuclear workers | 72 | 54 hours/week averaged over 6 weeks8 | N/A |
| Canadian Commercial Vehicle Drivers Hours of Service Regulations | Canadian motor carrier drivers | -1-wk cycle: 70 hrs in 7 days (Sec. 26) OR -2-wk cycle: 120 hrs on duty in 14 days or 24 consecutive hrs off duty after 70 hrs on-duty | N/A | N/A |
5N/A indicates that the legislation does not include this requirement
6Limits applicable to 7-day and 28-day period are also in EU Commission Regulation No. 83/2014 related to air operations
7Transport Canada is proposing new limits applicable to pilots that are similar to those of the US and EU (105).
8US NRC licensees may select a limit of 54 hours per week averaged over 6 weeks as an alternative to the requirements for a minimum number of days off.
Table 3: Benchmarking of limits on consecutive shifts and recovery periods
| Legislation | Type of Workers | Consecutive Shifts | Recovery Periods | Limits on Consecutive Night Shifts | Recovery Periods After Night Shifts |
|---|---|---|---|---|---|
| EU Working Time Directive | All EU workers including nuclear | N/A9 | Uninterrupted rest period of 35 hours per each 7-day period10 | N/A11 | N/A |
| 14 CFR Part 117 | US pilots | 30 consecutive hours free from duty in past 7 days | N/A | 3 nights that infringe on window of circadian low or 5 nights if rest opportunity of at least 2 hrs during each night time flight duty period | N/A |
| CNSC – in REGDOC-2.2.4, Volume I | SSPs, high-security sites | Up to 6 shifts >10 to 12 hours | N/A | 4 night shifts >10 hrs – 12 hrs | >10-12 hr night shifts: 48 hrs off after 2 nights; 72 hrs off after >3 nights |
| 5 night shifts 8–10 hrs | 8–10 hr night shifts: 48 hrs off after 4 or more | ||||
| US NRC – 10 CFR Part 26 | US nuclear workers | -8-hour shifts: 1 day off / week -10-hour shifts: 2 days off / week -12-hour shifts: 2 to 3 days off/wk12,13, (days off may be averaged over shift cycle) -34-hour break in any 9-day period12 | N/A | N/A |
9N/A indicates that the legislation does not include this requirement
10Table presents restrictions on consecutive shifts and recovery periods that exceed requirement in most jurisdictions for at least 24 hours off / 7-day period.
11The EU Working Time Directive includes the following restriction on night work: "normal hours of work for night workers do not exceed an average of eight hours in any 24-hour period".
12Recovery period requirements in US NRC 10 CFR Part 26 vary depending upon position (e.g., security – 3 days off; operations – 2.5 days off; maintenance – 2 days off per week averaged over shift cycle)
13US NRC day off requirements are reduced during outages (e.g., Operations – at least 3 days off in each successive 15-day period; maintenance – at least 1 day off in any 7 days); recovery period of 34 hours in any 9-day period is applicable at all times
2.2.7 Ranking of Limits on Hours of Work and Recovery Periods
Models that integrate scientific information about circadian rhythms, wakefulness and recovery periods are available to predict levels of fatigue (106; 107). The "strongest scientific basis of fatigue models is that they capture important fatigue trends", so they are a useful tool for comparing different work schedules for a workforce (107 p. 23).
CNSC staff applied the bio-mathematical model FAID, version 2.2.0.210 (2014), to various work schedules that are permissible and non-compliant with the REGDOC. FAID, which was developed by the Centre for Sleep Research at the University of South Australia, is a well-known model that is widely used, including in aviation in Canada and in rail in Australia (108; 109). Due to the limitations of fatigue models, the results from the review of work schedules using the FAID model have been considered as an adjunct to scientific literature and benchmarking (106; 107; 108; 110).
FAID software is based on a token economy. Fatigue tokens accumulate during work and recovery tokens accumulate during non-work periods (111). The fatigue value of work and recovery value of non-work periods are based on their length, circadian timing and how recently they occurred (111 p. A62). Using the model, "more recent work/non-work periods make a greater relative contribution to the overall fatigue score than less recent work/non-work periods" (111 p. A62). Based on validation activities with data collected in labs and workplace settings, the FAID model is able to discriminate between more and less demanding schedules (111).
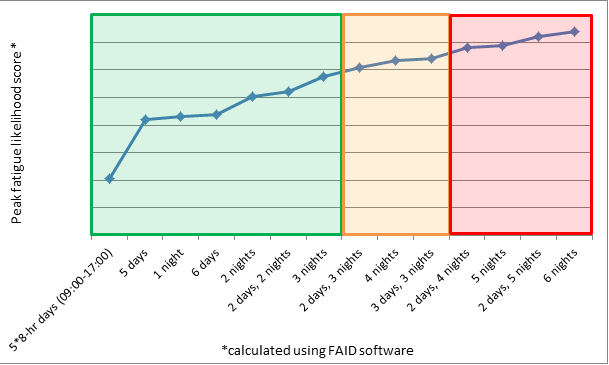
Figure 3: Rank ordering of limits in REGDOC as tested using fatigue model.
NOTE: The first data point shows peak fatigue predicted from 5 8-hour day shifts. The remaining data points are for shifts that are 12 hours long, plus 30 minutes for shift turnover. Day shifts are from 07:30 to 20:00 and night shifts are from 19:30 to 08:00.
Figure 3 shows peak fatigue scores associated with different shift sequences. The first and second boxes (green and orange) represent schedules that are permissible within the REGDOC. Schedules within the second box are permissible, but guidance highlights that these schedules should not be routine. The third box (red) represents schedules that would be non-compliant with the REGDOC.
3. Conclusions
The REGDOC includes a comprehensive suite of requirements and guidance for managing worker fatigue. These measures are intended to reduce the occurrence of high levels of fatigue and to reduce the likelihood and consequences of fatigue-related errors.
The requirements and guidance in the REGDOC are informed by scientific information about the effects of fatigue on human performance and on benchmarking with other regulatory bodies. In response to comments received during public consultation, the regulatory requirements have been modified to increase the focus on the highest risk aspects of shift work: extended shifts longer than 10 hours and night work. CNSC staff considered requests for revisions to the REGDOC received during public consultation in light of scientific information and benchmarking. Requests were also considered based on how they would affect the rank ordering of limits within the REGDOC, as shown in Figure 3.
CNSC staff will continue to monitor science and regulatory practices related to fatigue management and will consider any new information for incorporation into subsequent versions of the REGDOC.
References
- Dawson, D., Chapman, J. and Thomas, M. (2012). Fatigue-proofing: A new approach to reducing fatigue-related risk using the principles of error management. Sleep Medicine Reviews, 16, 167-175.
- Smiley, A. and Moray, N.P. (1989). Review of 12-hour Shifts at Nuclear Generating Stations. Ottawa: Atomic Energy Control Board, INFO-0318.
- Kulp, K. (1999). Development of a Regulatory Monitoring Program for Shiftwork Systems at Canadian Nuclear Power Plants. Ottawa: Atomic Energy Control Board, RSP-0096.
- Smiley, A. and Rudin-Brown, C. (2013). Review of Criteria for Assessing Shift Schedules in the Nuclear Industry. Ottawa: Canadian Nuclear Safety Commission, RSP-0289.
- Borbély, A. (1982). A two process model of sleep regulation. Human Neurobiology, 1(3), 195-204.
- Belenky, G., Wesensten, N., Thorne, D., Thomas, M., Sing, H., Redmond, D.,... Balkin, T. (2003). Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. Journal of Sleep Research, 12, 1-12.
- Van Dongen, H., Maislin, G., Mullington, J. and Dinges, D. (2003). The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep, 26(2), 117-126.
- Gander, P., Hartley, L., Powell, D., Cabon, P., Hitchcock, E., Mills, A. and Popkin, S. (2011). Fatigue risk management: Organizational factors at the regulatory and industry/company level. Accident Analysis and Prevention, 43, 573-590.
- Cohen, D., Wang, W., Wyatt, J., Kronauer, R., Dijk, D., Czeisler, C. and Klerman, E. (2010). Uncovering residual effects of chronic sleep loss on human performance. Science Translational Medicine, 2(14).
- Dijk, D., Duffy, J. and Czeisler, C. (1992). Circadian and sleep/wake dependent aspects of subjective alertness and cognitive performance. Journal of Sleep Research, 1, 112-117.
- Balkin, T., Rupp, T., Picchioni, D. and Wesensten, N. (2008). Sleep loss and sleepiness: Current issues. Contemporary Reviews in Sleep Medicine, 134(3), 653-660.
- Goel, N., Rao, H., Durmer, J. and Dinges, D. (2009). Neurocognitive consequences of sleep deprivation. Seminars in Neurology, 29(4), 320-339.
- Philibert, I. (2005). Sleep loss and performance in residents and nonphysicians: A meta-analytic examination. Sleep, 28(11), 1392-1402.
- Kryger, M., Roth, T. and Dement, W. (2011). Principles and Practice of Sleep Medicine (Fifth ed.). St. Louis: Elsevier Saunders.
- Matthews, G., et al. (2012). The Handbook of Operator Fatigue. Farnham: Ashgate Publishing Limited.
- Pilcher, J. and Huffcutt, A. (1996). Effects of sleep deprivation on performance: A meta-analysis. Sleep, 19(4), 318-326.
- Williamson, A., Lombardi, D., Folkard, S., Stutts, J., Courtney, T. and Connor, J. (2011). The link between fatigue and safety. Accident analysis and Prevention, 43, 498-515.
- Phillips, R. (2014). What is fatigue and how does it affect the safety performance of human transport operators? Fatigue in Transport Report 1. Oslo : Institute of Transport Economics, T01 report 1351/2014.
- Banks, S., Van Dongen, H., Maislin, G. and Dinges, D. (2010). Neurobehavioral dynamics following chronic sleep restriction: Dose-response effects of one night for recovery. Sleep, 33(8), 1013-1026.
- Bratzke, D., Rolk, B. and Peters, M. (2007). Central slowing during the night. Psychological Science, 18(5), 456-461.
- Drake, C., Roehrs, T., Burduvali, E., Bonahoom, A., Rosekind, M. and Roth, T. (2001). Effects of rapid versus slow accumulation of eight hours of sleep loss. Psychophysiology, 38, 979-987.
- Lim, J. and Dinges, D. (2010). A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychological Bulletin, 136(3), 375-389.
- Dinges, D., Pack, F., Williams, K., Gillen, K., Powell, J., Ott, G.,... Pack, A. (1997). Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep, 20(4), 267-277.
- Gohar, A., Adams, A., Gertner, E., Sackett-Lundeen, L., Heitz, R., Engle, R.,... Bijwadia, J. (2009). Working memory capacity is decreased in sleep-deprived internal medicine residents. Journal of Clinical Sleep Medicine, 5(3), 191-197.
- Johnson, M., Duffy, J., Dijk, D., Ronda, J., Dyal, C. and Czeisler, C. (1992). Short-term memory, alertness and performance: a reappraisal of their relationship to body temperature. Journal of Sleep Research, 1, 24-29.
- Walker, M. (2008). Sleep-dependent memory processing. Harvard Review of Psychiatry, 16, 287-298.
- Harrison, Y. and Horne, J. (2000). The impact of sleep deprivation on decision making: A review. Journal of Experimental Psychology: Applied, 6(3), 236-249.
- Venkatraman, V., Chuah, Y., Huettel, S. and Chee, M. (2007). Sleep deprivation elevates expectation of gains and attenuates response to losses following risky decisions. Sleep, 30(5), 603-609.
- Goldstein, A., Greer, S., Saletin, J., Harvey, A., Nitschke, J. and Walker, M. (2013). Tired and apprehensive: Anxiety amplifies the impact of sleep loss on aversive brain anticipation. The Journal of Neuroscience, 33(26), 10607-10615.
- Barger, L., Lockley, S., Rajaratnam, S. and Landrigan, C. (2009). Neurobehavioral, health, and safety consequences associated with shift work in safety-sensitive professions. Current Neurology and Neuroscience Reports, 9, 155-164.
- National Research Council. (2011). The Effects of Commuting on Pilot Fatigue. Washington, DC: The National Academies Press.
- Mitler, M., Carskadon, M., Czeisler, C., Dement, W., Dinges, D. and Graeber, R. (1988). Catastrophes, sleep and public policy: Consensus report. Sleep, 11(1), 100-109.
- Hobbs, A., Williamson, A. and Van Dongen, H. (2010). A circadian rhythm in skill-based errors in aviation maintenance. Chronobiology International, 27(6), 1304-1316.
- Heslegrave, R., Rhodes, W. and Gil, V. (2000). A prospective study examining the changes to worker health and safety after shifting from 9 to 12.5-hour shifts. In S. Hornberger, P. Knauth, G. Costa, & S. Folkard, Shiftwork in the 21st Century (pp. 175-180). Frankfurt: Peter Lang.
- Elliott, W. and Mein, D. (2001). Report of the Tripartite Steering Committee on ATC Fatigue. Ottawa: Transport Canada, Report No. TP-13742E.
- Lerman, S., Eskin, E., Flower, D., George, E., Gerson, B., Hartenbaum, N.,... Moore-Ede, M. (2012). Fatigue risk management in the workplace. Journal of Occupational and Environmental Medicine, 54(2), 231-258.
- Fletcher, A., Hooper, B., Dunican, I. and Kogi, K. (2015). Fatigue Management in Safety-Critical Operations: History, Terminology, Management System Frameworks, and Industry Challenges. Reviews of Human Factors and Ergonomics, 10, 6-28.
- International Civil Aviation Organization. (2011). Fatigue Management-related excerpts from: Annex 6 to the Convention on International Civil Aviation.
- Transport Canada. (2011). Development and Implementation of Fatigue Risk Management Systems in the Canadian Aviation Industry, Advisory Circular SUR-001.
- Safe Work Australia (2013). Guide for Managing the Risk of Fatigue at Work.
- Darwent, D., Dawson, D., Paterson, J., Roach, G. and Ferguson, S. (2015). Managing Fatigue: It really is about sleep. Accident Analysis, 82, 20-26.
- Smolensky, M., Di Milia, L., Ohayon, M., and Philip, P. (2011). Sleep disorders, medical conditions, and road accident risk. Accident Analysis and Prevention, 43, 533-548.
- Paim, S., Pires, M., Bittencourt, L., Silva, R., Santos, R., Esteves, A.,... de Mello, M. (2008). Sleep complaints and polysomnographic findings: A study of nuclear power plant shift workers. Chronobiology International, 25(2&3), 321-331.
- Tulio de Mello, M., Narciso, F., Tufik, S., Paiva, T., Spence, D., BaHammam, A. Pandi-Perumal, S. (2013). Sleep disorders as a cause of motor vehicle collisions. International Journal of Preventive Medicine, 4(3), 246-257.
- Richter, K., Acker, J., Adam, S. and Niklewski, G. (2016). Prevention of fatigue and insomnia in shift workers – a review of non-pharmacological measures. The EPMA Journal, 7, 16.
- Driskell, J. and Mullen, B. (2005). The efficacy of naps as a fatigue countermeasure: A meta-analytic integration. Human Factors, 47(2), 360-377.
- Tremaine, R., Dorrian, J., Lack, L., Lovato, N., Ferguson, S., Zhou, X. and Roach, G. (2010). The relationship between subjective and objective sleepiness and performance during a simulated night-shift with a nap countermeasure. Applied Ergonomics, 42, 52-61.
- Ficca, G., Axelsson, J., Mollicone, D., Muto, V. and Vitiello, M. (2010). Naps, cognition and performance. Sleep Medicine Reviews, 14, 249-258.
- Monk, T. (1986). Advantages and disadvantages of rapidly rotating shift schedules – A circadian viewpoint. Human Factors, 28(5), 553-557.
- Roach, G., Dawson, D. Reid, K., Darwent, D. and Sargent, C. (2016). The time-of-day that breaks occu between consecutive duty periods affects the sleep strategies used by shiftworkers. Chronobiology International, 33, 653-656.
- Dinges, D., Graeber, R., Rosekind, M., Samel, A. and Wegmann, H. (1996). Principles and Guidelines for Duty and Rest Scheduling in Commercial Aviation. Moffett Field: NASA Ames Research Center.
- Federal Aviation Administration, 14 CFR Part 117, Flight and duty limitations and rest requirements: Flightcrew members.
- Ferguson, S., Paech, G., Dorrian, J., Roach, G. and Jay, S. (2011). Performance on a simple response time task: Is sleep or work more important for miners. Applied Ergonomics, 42, 210-213.
- Scott, L., Rogers, A., Hwang, W. and Zhang, Y. (2006). Effects of critical care nurses' work hours on vigilance and patients' safety. American Journal of Critical Care, 15(1), 30-37.
- Watson, N., Badr, M., Belenky, G., Bilwise, D., Buxton, O., Buysse, D.... Tasali, E. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep, 38(6), 843-844.
- National Sleep Foundation. (2008). 2008 Sleep in America Poll. Washington: National Sleep Foundation.
- Vedaa, O., Harris, A., Bjorvatn, B., Waage, S., Sivertsen, B., Tucker, P. and Pallesen, S. (2016). Systematic review of the relationship between quick returns in rotating shift work and health-related outcomes. Ergonomics, 59(1), 1-14.
- Czeisler, C., Wickwire, E., Barger, L., Dement, W., Gamble, K., Hartenbaum, N.,... Hirshkowitz, M. (2016). Sleep-deprived motor vehicle operators are unfit to drive: a multidisciplinary expert consensus statement on drowsy driving. Sleep Health, 2(2), 94-99.
- Roach, G., Reid, K. and Dawson, D. (2003). The amount of sleep obtained by locomotive engineers: effects of break duration and time of break onset. Occupational and Environmental Medicine, 60(12), e17.
- Rosenthal, L., Roehrs, T., Rosen, A. and Roth, T. (1993). Level of sleepiness and total sleep time following various time in bed conditions. Sleep, 16(3), 226-232.
- Folkard, S., Robertson, K. and Spencer, M. (2007). A fatigue/risk index to assess work schedules. Somnologie, 11, 177-185.
- Eldevik, M., Flo, E., Moen, B., Pallesen, S. and Bjorvatn, B. (2013). Insomnia, excessive sleepiness, excessive fatigue, anxiety, depression and shift work disorder in nurses having less than 11 hours in-between shifts. PLOS ONE, 8, e70882.
- Dahlgren, A., Tucker, P., Gustavsson, P. and Rudman, A. (2016). Quick returns and night work as predictors of sleep quality, fatigue, work-family balance and satisfaction with work hours. Chronobiology International, 33, 759-767.
- Van Dongen, H. and Dinges, D. (2005). Sleep, circadian rhythms, and psychomotor vigilance. Clinical Sports Medicine, 24, 237-249.
- Wagstaff, A. and Sigstad, J. (2011). Shift and night work and long working hours – a systematic review of safety implications. Scandinavian Journal of Work and Environmental Health, 37(3), 173-185.
- Folkard, S. and Lombardi, D. (2006). Modeling the impact of the components of long work hours on injuries and "accidents". American Journal of Industrial Medicine, 49, 953-963.
- Knauth, P. (2007). Extended work periods. Industrial Health, 45, 125-136.
- Lamond, N. and Dawson, D. (1999). Quantifying the performance impairment associated with fatigue. Journal of Sleep Research, 8, 255-262.
- Doran, S., Van Dongen, H. and Dinges, D. (2001). Sustained attention performance during sleep deprivation: Evidence of state instability. Archives Italiennes de Biologie, 139, 253-267.
- Konowal, N., Van Dongen, H., Powell, J., Mallis, M. and Dinges, D. (1999). Determinants of microsleeps during experimental sleep deprivation. Sleep, 22S1, S328.
- Hale, L. (2005). Who has time to sleep? Journal of Public Health, 27(2), 205-211.
- Roenneberg, T., Kuehnle, T., Juda, M., Kantermann, T., Allebrandt, K., Gordijn, M. and Merrow, M. (2007). Epidemiology of the human circadian clock. Sleep Medicine Reviews, 11, 429-438.
- Basner, M., Fomberstein, K., Razavi, F., Banks, S., William, J., Rosa, R. and Dinges, D. (2007). American time use survey: Sleep time and its relationship to waking activities. Sleep, 30(9), 1085-1095.
- Tucker, P., Smith, L., Macdonald, I. and Folkard, S. (1999). Distribution of rest days in 12 hour shift systems: impacts on health, wellbeing, and on shift alertness. Occupational and Environmental Medicine, 56, 206-214.
- Paech, G., Jay, S., Lamond, N., Roach, G. and Ferguson, S. (2010). The effects of different roster schedules on sleep in miners. Applied Ergonomics, 41, 600-606.
- Geiger-Brown, J., Rogers, V., Trinkoff, A., Kane, R., Bausell, R. and Scharf, S. (2012). Sleep, sleepiness, fatigue and performance of 12-hour-shift nurses. Chronobiology International, 29(2), 211-219.
- Escriba, V., Perez-Hoyos, S. and Bolumar, F. (1992). Shiftwork: its impact on the length and quality of sleep among nurses of the Valencian region of Spain. Occupational and Environmental Health, 64(2), 125-129.
- Pilcher, J. and Huffcutt, A. (1996). Effects of sleep deprivation on performance: A meta-analysis. Sleep, 19(4), 318-326.
- Van Dongen, H., Rogers, N. and Dinges, D. (2003). Sleep debt: Theoretical and empirical issues. Sleep and Biological Rhythms, 1, 5-13.
- Mollicone, D., Van Dongen, H., Rogers, N., Banks, S. and Dinges, D. (2010). Time of day effects on neurobehavioral performance during chronic sleep restriction. Aviation, Space, and Environmental Medicine, 81, 735-744.
- Spencer, M., Robertson, K. and Folkard, S. (2006). The development of a fatigue/risk index for shift workers. Health and Safety Executive Report No. 446.
- Folkard, S. and Tucker, P. (2003). Shift work, safety and productivity. Occupational Medicine, 53, 95-101.
- Drake, C. and Wright, K. (2011). Shift work, shift-work disorder, and jet lag. In M. Kryger, T. Roth and W. Dement, Principles and Practice of Sleep Medicine (pp. 784-798). St. Louis: Elsevier Saunders.
- Monk, T., Folkard, S. and Wedderburn, A. (1996). Maintaining safety and high performance on shiftwork. Applied Ergonomics, 27(1), 17-23.
- Totterdell, P., Spelten, E., Smith, L., Barton, J. and Folkard, S. (1995). Recovery from work shifts: How long does it take? Journal of Applied Psychology, 80(1), 43-57.
- Akerstedt, T., Ingre, M., Kecklund, G., Folkard, S. and Axelsson, J. (2008). Accounting for partial sleep deprivation and cumulative sleepiness in the three-process model of alertness regulation. Chronobiology International, 25(2&3), 309-319.
- Akerstedt, T., Kecklund, G., Gillberg, M., Lowden, A. and Axelsson, J. (2000). Sleepiness and days of recovery. Transportation Research Part F 3, 251-261.
- Atomic Energy Control Board, Directorate of Analysis & Assessment and Directorate of Reactor Regulation (1994). Ontario Hydro Trial 12-hour Shiftworking. BMD 94-173, e-doc 3004687.
- Folkard, S. (2008). Do permanent night workers show circadian adjustment? A review based on the endogenous melatonin rhythm. Chronobiology International, 25(2&3), 215-224.
- Virtanen, M., Ferrie, J., Gimeno, D., Vehtera, J., Elovainio, M., Singh-Manoux, A.,... Kivimaki, M. (2009). Long working hours and sleep disturbances: The Whitehall II prospective cohort study. Sleep, 32(6), 737-745.
- Lombardi, D., Folkard, S., Willetts, J. and Smith, G. (2010). Daily sleep, weekly working hours, and risk of work-related injury: US national health interview survey (2004-2008). Chronobiology International, 27(5), 1013-1030.
- Dembe, A., Erickson, J., Delbos, R. and Banks, S. (2005). The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occupational and Environmental Medicine, 588-597.
- Vegso, S., Cantley, L., Slade, M., Taiwo, O., Sircar, K., Rabinowitz, P.,... Cullen, M. (2007). Extended work hours and risk of acute occupational injury: A case-crossover study of workers in manufacturing. American Journal of Industrial Medicine, 597-603.
- Dong, X. (2005). Long workhours, work scheduling and work-related injuries among construction workers in the United States. Scandinavian Journal of Work and Environmental Health, 31(5), 329-335.
- Stutts, J., Wilkins, J., Osberg, J. and Vaughn, B. (2003). Driver risk factors for sleep-related crashes. Accident Analysis and Prevention, 35, 321-331.
- Rogers, A., Hwang, W., Scott, L., Aiken, L. and Dinges, D. (2004). The working hours of hospital staff nurses and patient safety. Health Affairs, 202-212.
- Cappuccio, F., Bakewell, A., Taggart, F., Ward, G., Sullivan, J., Edmunds, M.,... Peile, E. (2009). Implementing a 48 h EWTD-compliant rota for junior doctors in the UK does not compromise patients' safety: assessor-blind pilot comparison. The Quarterly Journal of Medicine, 102, 271-282.
- Landrigan, C., Rothschile, J., Cronin, J., Kaushal, R., Burdick, E., Katz, J.,... Czeisler, C. (2004). Effect of reducing interns' work hours on serious medical errors in intensive care units. The New England Journal of Medicine, 351, 1838-1848.
- Federal Aviation Administration. (2011). Flightcrew Member Duty and Rest Requirements, RIN 2120-AJ58.
- Deloitte Centre for Strategy & Evaluation Services. (2010). Study to support an Impact Assessment on further action at European level regarding Directive 2003/88/EC and the evolution of working time organization, Annex 1 – Study on health and safety aspects of working time. European Commission DG for Employment, Social Affairs and Equal Opportunities.
- U.S. Federal Register. (2008). Nuclear Regulatory Commission, 10 CFR Part 26, 73(62), 16966-17235.
- International Labour Organization. C014 – Weekly Rest (Industry) Convention, 1921 (No. 14).
- The European Parliament and the Council of the European Union. (2003). Directive 2003/88/EC of the European Parliament and of the Council of 4 November 2003 concerning certain aspects of the organisation of working time.
- International Labour Organization. (1990). R178 – Night Work Recommendation.
- Transport Canada. (2014). Canadian Aviation Regulation Advisory Council (CARAC) Notice of Proposed Amendment (NPA): Flight Crew Fatigue Management, CARAC Activity Reporting Notice 2014-019. Ottawa: Transport Canada.
- Dawson, D., Noy, Y., Harma, M., Akerstedt, T. and Belenky, G. (2011). Modelling fatigue and the use of fatigue models in work settings. Accident Analysis and Prevention, 43, 549-564.
- Civil Aviation Safety Authority Australia. (2014). Biomathematical Fatigue Models Guidance Document. Albert Park: Civil Aviation Safety Authority.
- Independent Transport Safety Regulator Australia. (2010). Transport Safety Alert – Use of bio-mathematical models in managing risks of human fatigue in the workplace. Independent Transport Safety Regulator, TSA no. 34.
- Transport Canada. (2011). Development and Implementation of Fatigue Risk Management Systems in the Canadian Aviation Industry, Advisory Circular SUR-001. Ottawa: Transport Canada.
- Australian Transport Safety Bureau (2011). Signal passed at danger by train ST24 Junee, New South Wales 9 September 2009. Canberra : Australian Transport Safety Bureau, RO-2009-008.
- Roach, G., Fletcher, A. and Dawson, D. (2004). A model to predict work-related fatigue based on hours of work. 75(3), A61-A69.
Page details
- Date modified: